“The greatest threat to human health in the 21st century is the rise of drug-resistant bacteria.” – Dr. Margaret Chan, Former Director-General of the World Health Organization.
Drug-resistant bacteria, or “superbugs,” are a big concern for our health. The U.S. Centers for Disease Control and Prevention (CDC) says these bacteria infect over 2 million people yearly. This leads to at least 23,000 deaths. We need a strong plan to fight antibiotic resistance.
Antibiotic Resistance: Fact-Checked Snapshot From Official Sources
- Annual U.S. Impact: Over 2.8 million antibiotic-resistant infections and 35,000+ deaths in the U.S. yearly. (CDC)
- Global Prevalence: 1 in 6 bacterial infections worldwide are now resistant to antibiotics. Highest rates seen in South-East Asia and Eastern Mediterranean. (WHO Surveillance 2025)
- Top ‘Superbugs’: Includes E. coli, MRSA (S. aureus), Klebsiella, Acinetobacter and others. (Review)
- Economic Burden: Over $4.6 billion/year in U.S. healthcare costs for AR germs. (CDC)
- Latest Trends: WHO warns of rising resistance in over 40% of pathogen-antibiotic pairs worldwide. (WHO News Oct 2025)

What You Must Know About Superbugs
Understanding Antimicrobial Resistance and Its Global Health Impact
Superbugs—microorganisms resistant to multiple antimicrobial agents—represent one of the most pressing global health threats of the 21st century. The World Health Organization estimates that antimicrobial resistance (AMR) could cause 10 million deaths annually by 2050 if left unchecked, surpassing cancer as a leading cause of mortality. Understanding superbugs is no longer optional for healthcare professionals, researchers, and the general public—it is essential for protecting individual and public health. This comprehensive guide presents critical facts about superbugs that everyone should know.
Superbugs Are Not a Single Organism—They Are a Growing Family of Resistant Pathogens
The term “superbug” encompasses diverse microorganisms—bacteria, fungi, viruses, and parasites—that have developed resistance to antimicrobial drugs designed to eliminate them. The most clinically significant superbugs include MRSA (Methicillin-Resistant Staphylococcus aureus), which causes severe skin, bloodstream, and surgical site infections resistant to beta-lactam antibiotics; VRE (Vancomycin-Resistant Enterococcus), particularly problematic in hospitalized and immunocompromised patients; CRE (Carbapenem-Resistant Enterobacteriaceae), often called “nightmare bacteria” with mortality rates exceeding 50% in bloodstream infections; MDR-TB (Multidrug-Resistant Tuberculosis) and XDR-TB (Extensively Drug-Resistant Tuberculosis), requiring 18-24 months of toxic, expensive treatment; Candida auris, a multidrug-resistant fungal pathogen spreading globally in healthcare settings; and Neisseria gonorrhoeae strains resistant to all first-line antibiotics, threatening untreatable sexually transmitted infections.
Critical Insight: The WHO Priority Pathogens List identifies 12 bacterial families posing the greatest threat to human health, with carbapenem-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacteriaceae classified as “critical priority” requiring urgent research and development of new antibiotics.
Antimicrobial Resistance Is Driven by Multiple Interconnected Factors
Superbug emergence results from complex interactions between human behavior, medical practices, and evolutionary biology. Inappropriate antibiotic use remains the primary driver—prescribing antibiotics for viral infections (which they cannot treat), incomplete treatment courses allowing resistant bacteria to survive, and patient self-medication without proper diagnosis. Agricultural misuse contributes significantly, with approximately 73% of global antimicrobials used in livestock for growth promotion and disease prevention, creating resistant bacteria that transfer to humans through food chains and environmental contamination. Healthcare-associated transmission occurs through inadequate infection control, contaminated medical devices, and high-density patient populations facilitating pathogen spread. Global travel and trade enable rapid international dissemination of resistant strains across continents within hours.
Environmental Factors: Pharmaceutical manufacturing waste, hospital effluents, and agricultural runoff containing antibiotic residues create environmental reservoirs where bacteria exchange resistance genes. Wastewater treatment plants often fail to remove antibiotics completely, contributing to resistance development in aquatic ecosystems and soil microbiomes.
Bacteria Share Resistance Genes Through Horizontal Gene Transfer
Unlike humans who inherit genes only from parents, bacteria can acquire resistance genes from completely unrelated species through three mechanisms of horizontal gene transfer (HGT). Conjugation involves direct cell-to-cell contact where plasmids (circular DNA molecules) carrying multiple resistance genes transfer between bacteria, even across species boundaries—a single plasmid can confer resistance to 5-10 different antibiotics simultaneously. Transformation occurs when bacteria absorb free DNA from dead bacterial cells in their environment, incorporating resistance genes into their own genome. Transduction uses bacteriophages (viruses that infect bacteria) as vehicles to transfer resistance genes between bacterial cells.
Clinical Implications: This genetic promiscuity means resistance can spread rapidly within bacterial communities in the human gut, on hospital surfaces, or in environmental reservoirs. A harmless gut bacterium can transfer resistance genes to pathogenic bacteria, creating superbugs without direct antibiotic exposure. This phenomenon explains why resistance can emerge in bacteria that have never encountered specific antibiotics.
The Antibiotic Pipeline Is Dangerously Depleted
While resistance accelerates, new antibiotic development has dramatically declined—no new classes of antibiotics have been discovered since the 1980s. The pharmaceutical industry has largely abandoned antibiotic research due to unfavorable economics: antibiotics are used for short durations (unlike chronic disease medications), resistance develops quickly (shortening a drug’s useful lifespan), regulatory requirements are stringent and expensive, and return on investment is poor compared to other therapeutic areas. Between 2000 and 2020, only 2-3 new systemic antibacterial agents were approved annually, compared to 16 new antibiotics approved in the 1980s alone.
Current Pipeline Status: As of 2024, approximately 60 antibiotics are in clinical development, but most are derivatives of existing classes with limited activity against priority pathogens. Only 6-8 candidates target WHO critical priority pathogens. Many small biotech companies developing innovative antibiotics face bankruptcy despite successful drug development, as market dynamics cannot sustain antibiotic innovation without new economic models or government intervention.
Superbugs Disproportionately Impact Vulnerable Populations and Healthcare Systems
Antimicrobial resistance creates devastating health and economic consequences, particularly for vulnerable groups. Healthcare burden: Superbug infections increase hospital stays by 7-14 days, require more expensive second- and third-line antibiotics, necessitate intensive care admission more frequently, and result in mortality rates 2-3 times higher than susceptible infections. Economic impact: The World Bank estimates AMR could reduce global GDP by 1.1-3.8% by 2050, costing the global economy $100 trillion cumulatively. Individual patients face catastrophic healthcare costs—treating MDR-TB costs $250,000-$500,000 per patient compared to $2,000 for drug-susceptible TB.
Vulnerable Populations: Neonates, elderly patients, immunocompromised individuals (cancer patients, transplant recipients, HIV patients), surgical patients, and those with chronic diseases face highest risk. Low- and middle-income countries bear disproportionate burden due to limited access to diagnostics, inadequate infection control infrastructure, higher rates of counterfeit antibiotics, and greater environmental contamination.
Antimicrobial Stewardship Is Essential for Preserving Antibiotic Effectiveness
Antimicrobial stewardship programs (ASPs) implement evidence-based interventions to optimize antibiotic use, improving patient outcomes while minimizing resistance development. Core ASP strategies include prospective audit and feedback where infectious disease specialists review antibiotic prescriptions and provide recommendations; formulary restriction and preauthorization requiring approval for broad-spectrum or last-resort antibiotics; dose optimization ensuring adequate drug concentrations while minimizing toxicity and resistance selection; de-escalation protocols narrowing antibiotic spectrum based on culture results; and duration optimization using shortest effective treatment courses (e.g., 5-7 days for many infections previously treated for 10-14 days).
Evidence of Effectiveness: Well-implemented ASPs reduce inappropriate antibiotic use by 20-30%, decrease Clostridioides difficile infections by 30-50%, reduce healthcare costs by $200,000-$900,000 annually per hospital, and improve patient outcomes without increasing mortality. Rapid diagnostic technologies (PCR, MALDI-TOF mass spectrometry, next-generation sequencing) enable faster pathogen identification and targeted therapy, supporting stewardship efforts.
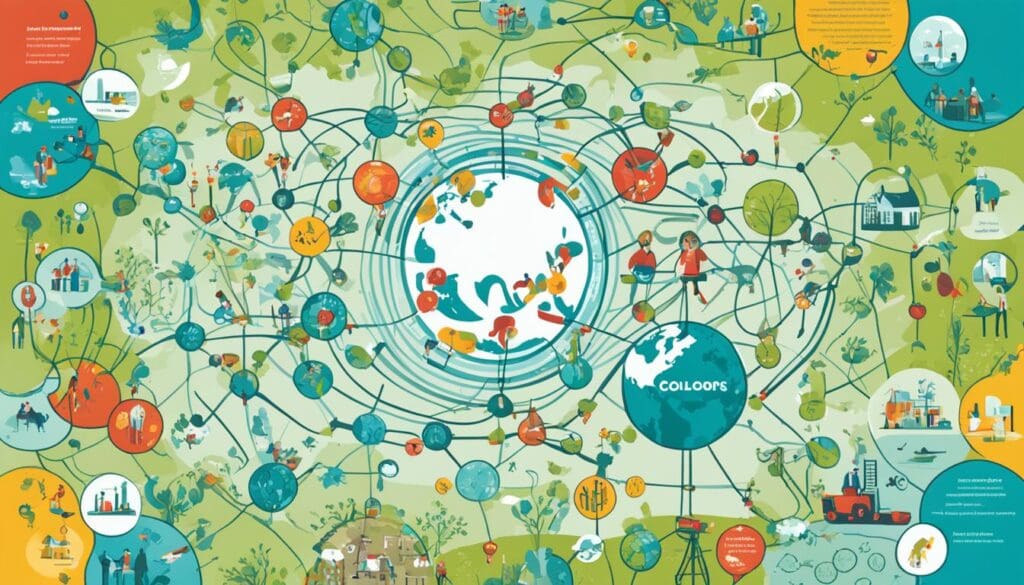
Everyone Has a Role in Combating Antimicrobial Resistance
Addressing superbugs requires coordinated action across multiple sectors—a “One Health” approach recognizing interconnections between human, animal, and environmental health. Healthcare professionals must prescribe antibiotics judiciously, implement infection prevention protocols, participate in stewardship programs, and educate patients about appropriate antibiotic use. Researchers and academics should prioritize AMR research, develop novel therapeutics (antibiotics, bacteriophages, immunotherapies, antimicrobial peptides), improve diagnostics, and publish findings to advance global knowledge. Policymakers must strengthen surveillance systems, regulate agricultural antibiotic use, incentivize antibiotic development through push/pull mechanisms, and ensure access to quality antibiotics globally.
Individual Actions: The public can combat resistance by never demanding antibiotics for viral infections, completing prescribed antibiotic courses as directed (not stopping when feeling better), never sharing or using leftover antibiotics, practicing good hygiene (handwashing prevents infections requiring antibiotics), getting recommended vaccinations (preventing infections reduces antibiotic need), and choosing antibiotic-free meat when possible. These seemingly small actions collectively create significant impact when practiced by millions.
Publishing Research on Antimicrobial Resistance?
Editverse provides comprehensive support for researchers working on AMR, infectious diseases, and microbiology, including manuscript writing, publication support, statistical analysis, and professional editing services to help your research reach high-impact journals.
Disclaimer: Information provided is for educational purposes only. While we strive for accuracy, Editverse disclaims responsibility for decisions made based on this information, accuracy of third-party sources, or any consequences of using this content. Readers are advised to verify information from primary sources and consult relevant experts.
For any inaccuracies or errors, please contact co*****@*******se.com
Last Updated: October 28, 2025
Key Takeaways
- Antibiotic resistance is a growing global threat, with drug-resistant “superbugs” infecting over 2 million people and killing at least 23,000 in the U.S. each year.
- Superbugs are strains of bacteria, viruses, parasites, or fungi that have developed resistance to many or most antibiotics, often due to overuse and misuse of these essential medications.
- Combating antibiotic resistance requires improved antimicrobial stewardship, enhanced infection prevention and control measures, development of novel antibiotics, and global collaboration on public health initiatives.
- The overuse and misuse of antibiotics in human healthcare and livestock production contribute to the creation of drug-resistant bacteria.
- Strategies to combat superbugs include promoting antimicrobial stewardship, enhancing infection prevention and control, supporting the development of new antibiotics, and implementing a One Health approach for global collaboration.
Understanding Antibiotic Resistance
Antibiotic resistance is a big worry for our health. It makes it hard to treat many infections. Superbugs are the main cause. They are bacteria, viruses, parasites, or fungi that don’t get better with most antibiotics.
These superbugs get stronger over time. They change and adapt to antibiotics. This happens because they keep getting exposed to these drugs.
What are Superbugs?
Superbugs are a big threat. Some of the worst ones include Escherichia coli (E. coli), Staphylococcus aureus (S. aureus), Klebsiella pneumoniae (K. pneumoniae), Streptococcus pneumoniae (S. pneumoniae), Acinetobacter baumannii (A. baumannii), and Pseudomonas aeruginosa. These superbugs also include C. diff (Clostridioides difficile), drug-resistant gonorrhea, MRSA (Methicillin-resistant Staphylococcus aureus), MDR-TB (Multi-drug-resistant Myobacterium tuberculosis), and Vancomycin-resistant Enterococci.
How Superbugs Develop Resistance
Antibiotic resistance comes from many factors. Misusing antibiotics is a big part of the problem. Giving antibiotics to animals that don’t need them helps spread these resistant germs.
When bacteria face antibiotics often, they change to survive. They develop new traits that make them resistant. This means antibiotics that used to work no longer do.
| Statistic | Percentage |
|---|---|
| Nearly all strains of Staphylococcus aureus in the United States are resistant to penicillin. | 100% |
| Since 1997, strains of S. aureus have been reported to have a decreased susceptibility to vancomycin. | N/A |
| One out of six cases of Campylobacter infections is resistant to fluoroquinolones. | 16.67% |
We need to understand how superbugs spread to fight them. To stop this, we should all practice good hygiene. Use antibiotics only when really needed. Get vaccines and see doctors for infections that don’t respond to antibiotics.
Antibiotic resistance is a global public health problem affecting everyone.
The Threat of Superbugs
Prevalence and Impact of Superbugs
The rise of superbug infections is a big threat to our health. These tough germs cause over 2 million infections and 23,000 deaths every year in the U.S. alone. Healthcare-associated infections and community-acquired infections are serious, leading to more illnesses and deaths. They also put a big strain on our wallets.
Superbugs are spreading beyond hospitals now. They’re showing up in everyday infections, making it harder to treat common illnesses. This means our ability to fight off many diseases is at risk. It’s a big problem for modern medicine.
| Metric | Impact |
|---|---|
| Infection Rates | Antibiotic-resistant bacteria infect at least 2.8 million Americans each year. |
| Mortality Rates | At least 35,000 Americans die annually due to antibiotic-resistant bacteria. |
| Economic Impact | Drug-resistant bacteria infections cost the U.S. healthcare system an estimated $20 billion each year. |
The danger from superbugs is clear. We need a strong plan to fight this issue. It will take work from doctors, lawmakers, and us, the public. We must act to protect our health and well-being.
Common Superbug Strains
As we face the threat of antibiotic resistance, some superbug strains are especially worrying. These include methicillin-resistant Staphylococcus aureus (MRSA), drug-resistant tuberculosis, gonorrhea, and the fungus Candida auris. These pathogens resist many or most antibiotics, making treatment hard.
But the problem isn’t just with bacteria. Drug-resistant viruses, parasites, and fungi are also superbugs, threatening human health. We need a wide-ranging plan to fight antimicrobial resistance.
Studies show that superbugs like MRSA are becoming more common, affecting about 10% of hospital patients. In the U.S., over 23,000 people die each year from infections caused by these resistant bacteria.
Superbugs are also spreading in everyday life, with healthy people getting infected more often. The use of antibiotics in farming is also a problem, making superbugs in animals a risk to food safety and public health.
The drug-resistant fungus Candida auris is a big worry, found in 28 states in the past year. This highlights the need for careful watch and teamwork to tackle superbugs in various areas and among different groups.
Causes of Antibiotic Overuse
The overuse and misuse of antibiotics are major reasons for antimicrobial resistance and superbugs. Many antibiotics are given out too freely, like for viral infections that don’t need them. Also, using antibiotics in farming, often to prevent disease and make animals grow bigger, helps spread resistant bacteria to humans.
Unnecessary Prescriptions
Studies say that 30% to 50% of antibiotic use is wrong, often because of bad treatment plans. In ICUs, 30% to 60% of antibiotics given out are not needed or are not the right choice, showing a big problem in critical care.
Misuse in Livestock
About 80% of antibiotics sold in the U.S. go to livestock, mainly for making animals grow bigger and preventing infections. These resistant bacteria can move from farm animals to people through meat, spreading antibiotic resistance to humans.
We need to work on better antimicrobial stewardship in both healthcare and farming to stop superbugs from growing.
“About one-third of antibiotic use in people is not needed nor appropriate, according to the Centers for Disease Control and Prevention.”
Wrong use of antibiotics leads to more health issues, like longer illnesses, more hospital stays, and higher costs. Using antibiotics right helps keep them working, protects against antibiotic-resistant infections, and reduces side effects.
Antibiotic Resistance: Combating Superbugs
To fight antibiotic resistance and superbugs, we need a strong plan. This plan includes using antibiotics wisely, creating new drugs, and improving how we prevent infections. Working together globally on health issues is also key. By tackling the main causes of resistance and using proven methods, we can keep antibiotics working and protect our health for the future.
Antimicrobial stewardship is a big part of fighting superbugs. It means doctors only give antibiotics when really needed. This helps stop bacteria from becoming resistant. Bacteria like MRSA and C. diff are very dangerous and hard to treat because they’re resistant to many antibiotics.
| Superbug Type | Prevalence and Impact |
|---|---|
| MRSA | Rates in hospitals are decreasing, but it remains a major concern |
| C. diff | Almost 30,000 deaths annually in the U.S., with many infections being resistant to common antibiotics |
| Antibiotic-resistant gonorrhea | About half of 1.6 million new cases annually are resistant to at least one antibiotic |
| Multidrug-resistant tuberculosis (MDR-TB) | Over 500,000 new cases reported in 2017, with extensively drug-resistant tuberculosis (XDR-TB) being even more resistant |
New ways like phage therapy also show promise against resistant bacteria. Phage therapy uses viruses to target and kill specific bacteria. It has helped make some tough infections more treatable.
“Phage therapy is considered a renewed approach to combat antibiotic-resistant bacteria.”
By using a comprehensive strategy, we can fight superbugs effectively. This means using antibiotics wisely, creating new drugs, improving infection control, and trying new treatments. Together, we can protect our health from these growing threats.
Strategies to Combat Superbugs
Fighting antibiotic resistance and superbugs needs a strong plan. Key steps include using antimicrobial stewardship programs and better infection control.
Antimicrobial Stewardship
Antimicrobial stewardship means setting and sharing antibiotic prescribing guidelines. It teaches healthcare workers, watches antibiotic use, and stops overuse. This way, we slow down drug-resistant bacteria growth and keep antibiotics working.
Infection Prevention and Control
Infection prevention and control are key to fighting superbugs. They focus on hand hygiene, strict cleaning and disinfection, and right use of PPE. This helps stop the spread of drug-resistant bacteria in hospitals and communities.
“Antimicrobial stewardship and infection prevention are essential strategies to address the growing threat of healthcare-associated infection reduction and antibiotic resistance.”
By using these proven methods together, we can fight superbugs and keep people safe. We need to stay alert, work together, and find new solutions to beat antibiotic resistance.
Novel Antibiotic Development
We need to work together to fight antibiotic resistance. But, finding new antibiotics has slowed down. There are scientific, regulatory, and economic hurdles. Researchers are looking at new ways to find effective antibiotics.
Overcoming Barriers to Antibiotic Discovery
One big challenge is understanding how bacteria become resistant. Researchers are finding new ways to target resistance. For example, they’re looking at how to block bacterial resistance pathways.
This could make antibiotics work better, like carbapenems. New antibiotic development is complex, but it’s crucial.
There are also regulatory hurdles in pharmaceutical research. Policymakers and industry leaders are trying to make things easier. They want to encourage innovation and speed up the approval process for new antibiotics.
We need to expand the antibiotic pipeline to fight superbugs. By using new strategies, like targeting resistance and combining treatments, we can make progress. Working together is key to finding new antibiotics and protecting public health from antibiotic resistance.
Alternative Therapies and Approaches
The global crisis of antibiotic resistance is getting worse. Researchers are looking into new ways to fight superbugs. They want to add more options to the fight against drug-resistant infections.
Phage therapy is one new idea. It uses viruses that target and kill bacteria. This method could help treat infections that traditional antibiotics can’t handle.
Antimicrobial peptides are another area of study. These are natural substances that can harm bacteria. They work by breaking down the bacteria’s cell walls and stopping them from working right.
Monoclonal antibodies are also being looked at. These are made to fight off pathogens and boost the immune system. They could help the body fight infections better.
Immune-modulating treatments are getting more attention too. Things like cytokine therapies and vaccines can help strengthen the immune system. This can make it easier to fight off infections, even those caused by resistant bacteria.
Researchers are also testing combination therapies. This means using antibiotics with other treatments. This could make treatments more effective against resistant infections.
As we face the threat of superbugs, exploring these new alternative antimicrobial therapies gives us hope. It could lead to a wider range of ways to fight antibiotic-resistant infections.
Global Collaboration and Public Health Initiatives
Fighting antibiotic resistance worldwide needs teams working together from all over. The World Health Organization’s Global Antimicrobial Resistance and Use Surveillance System (GLASS) tracks resistance patterns. It helps make important policy choices. The One Health approach brings together human, animal, and environmental health experts. They work together to fight antibiotic resistance in all areas.
Improving global monitoring, starting infection control programs, and working together across different fields is key. The Pan American Health Organization (PAHO) is helping countries in Latin America and the Caribbean fight antibiotic resistance. They are supporting the creation and use of national action plans on antibiotic resistance (AMR).
One Health Approach
PAHO is boosting surveillance in the Latin American and Caribbean region. This helps spot drug-resistant germs and see how they react to antibiotics. The group also runs training for health workers in the region on how to manage antibiotics wisely.
With ongoing support, countries in the region are getting better at stopping and handling new superbugs. Working together across different areas and using the “One Health” method is vital in fighting AMR worldwide.
| Key Initiatives | Impact |
|---|---|
| PAHO’s support for national AMR action plans in LAC countries | A third of the LAC countries have developed national action plans in line with the global objectives for combating AMR. |
| Strengthening regional surveillance systems | Improved ability to accurately identify drug-resistant pathogens and their antimicrobial susceptibility. |
| Training workshops on antimicrobial stewardship | Increased capacity of health professionals in the LAC region to implement effective antibiotic resistance prevention and control measures. |
“Multisectoral collaboration and a ‘One Health’ approach are crucial in combating AMR globally.”
Conclusion
The fight against antibiotic resistance and superbugs is a major global health issue. We must all be committed to it. The danger from drug-resistant germs is huge, with an estimated 700,000 deaths worldwide each year due to antimicrobial resistance. By 2050, we could lose $100 trillion because of this.
To beat this crisis, we need a full plan. This includes careful use of antibiotics, new antimicrobial research, better infection control, and working together globally on health issues. If we join forces, we can stop the spread of superbugs and keep our medicines working.
New treatments like phage therapy and CRISPR-enhanced treatments look promising against antibiotic-resistant infections. But, we need more research, trials, and approval before they can be used widely. The path ahead is tough, but if we stay focused, we can defeat superbugs and make a healthier world for everyone.
FAQ
What are superbugs?
Superbugs are types of bacteria, viruses, parasites, or fungi that resist many antibiotics and drugs. They’ve become resistant to these important medicines.
How do superbugs develop resistance?
Superbugs get resistant over time by changing and adapting to antibiotics. This happens because of too many antibiotics used, misuse in animals, and not enough new antibiotics being made.
What is the impact of superbugs?
More people are getting infections from superbugs, leading to more sickness and death. These infections also cost more to treat. They make treatments and procedures riskier.
What are some of the most concerning superbug strains?
Strains like methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant tuberculosis are very worrying. They resist many antibiotics, making them hard to treat.
What are the primary drivers of antibiotic resistance and superbug development?
Antibiotics are used too much and not always needed, which leads to resistance. Antibiotics given to animals also contribute to the problem.
What strategies are used to combat superbugs?
To fight superbugs, we use good antibiotic use programs, better infection control, and new antibiotics. Working together worldwide and through health initiatives is also key.
What are antimicrobial stewardship programs?
These programs create rules for using antibiotics right. They teach and watch over doctors to use them wisely. This slows down the spread of resistant bacteria.
What challenges are there to developing new antibiotics?
Making new antibiotics is hard because of science, rules, and money issues. Researchers are trying new ways, like targeting resistance and using the body’s own bacteria, to find solutions.
What are some alternative therapies and approaches to combat superbugs?
Scientists are looking at new treatments like phage therapy and immune system helpers. Using these new ideas with traditional antibiotics might help fight superbugs better.
How does the One Health approach help combat antibiotic resistance?
The One Health approach connects human, animal, and environment health. It encourages working together across fields to fight antibiotic resistance. This includes better tracking, infection control, and teamwork.
Source Links
- https://newsinhealth.nih.gov/2014/02/stop-spread-superbugs – Stop the Spread of Superbugs
- https://news.harvard.edu/gazette/story/2024/02/potential-new-weapon-in-battle-against-superbugs/ – Potential new weapon in battle against superbugs — Harvard Gazette
- https://www.nih.gov/news-events/nih-research-matters/designing-new-antibiotic-combat-drug-resistance – Designing a new antibiotic to combat drug resistance
- https://health.mo.gov/safety/antibioticresistance/generalinfo.php – What is Antibiotic Resistance | Antibiotic Resistance
- https://my.clevelandclinic.org/health/articles/21655-antibiotic-resistance – What Is Antibiotic Resistance?
- https://carb-x.org/news/antibiotic-resistance/ – Antibiotic Resistance – Carb-X
- https://www.mayoclinic.org/diseases-conditions/infectious-diseases/expert-answers/superbugs/faq-20129283 – Protect yourself from superbugs
- https://www.pewtrusts.org/en/trust/archive/winter-2022/superbugs-a-global-health-threat – Superbugs: A Global Health Threat
- https://newsinhealth.nih.gov/2023/10/stamping-out-superbugs – Stamping Out Superbugs
- https://www.aftermath.com/content/superbug-infection-bacteria/ – 5 Common Superbug Infections | Aftermath Services
- https://www.uhhospitals.org/blog/articles/2023/04/superbugs-are-surging-and-so-is-antibiotic-resistance – ‘Superbugs’ Are Surging and So Is Antibiotic Resistance
- https://www.antibioticresearch.org.uk/about-antibiotic-resistance/bacterial-infections/superbugs/ – Superbugs and Antibiotic Resistance | Resistant Infections
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/ – The Antibiotic Resistance Crisis: Part 1: Causes and Threats
- https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/antibiotics/art-20045720 – Antibiotics: Are you misusing them?
- https://www.goodrx.com/health-topic/infections/superbugs-and-antibiotic-resistance – Antibiotic Resistance and Superbugs – GoodRx
- https://www.ibiology.org/microbiology/fighting-antibiotic-resistance-with-phage-therapy/ – How to Kill a Superbug: Fighting antibiotic resistance with Phage Therapy • iBiology
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/your-role-in-stopping-superbugs – Your role in stopping ‘superbugs’
- https://www.pewtrusts.org/en/research-and-analysis/articles/2021/01/14/4-key-priorities-for-fighting-superbugs-in-2021 – 4 Key Priorities for Fighting Superbugs in 2021
- https://www.cnn.com/2024/01/03/health/new-antibiotic-drug-resistant/index.html – New antibiotic uses novel method to target deadly drug-resistant bacteria, study says | CNN
- https://www.ox.ac.uk/news/2024-05-03-novel-triple-drug-combination-effective-against-antibiotic-resistant-bacteria – Novel triple drug combination effective against antibiotic-resistant bacteria
- https://www.mdpi.com/1422-0067/21/3/1061 – Defeating Antibiotic-Resistant Bacteria: Exploring Alternative Therapies for a Post-Antibiotic Era
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9633024/ – Current Treatment Strategies Against Multidrug-Resistant Bacteria: A Review
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7870489/ – Futuristic Non-antibiotic Therapies to Combat Antibiotic Resistance: A Review
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7855710/ – Commentary: Microbial Resistance Movements: An Overview of Global Public Health Threats Posed by Antimicrobial Resistance, and How Best to Counter
- https://www.pewtrusts.org/en/research-and-analysis/articles/2018/12/13/international-efforts-critical-to-global-fight-against-superbugs – International Efforts Critical to Global Fight Against Superbugs
- https://bnrc.springeropen.com/articles/10.1186/s42269-023-01036-7 – Superbugs: a constraint to achieving the sustainable development goals – Bulletin of the National Research Centre
- https://www.scientificamerican.com/article/dangerous-superbugs-are-a-growing-threat-and-antibiotics-cant-stop-their-rise-what-can/ – Dangerous ‘Superbugs’ Are on the Rise. What Can Stop Them?