Imagine a medical system where one person receives a life-saving organ in a matter of weeks, while another faces an 18 to 24-month delay for the same procedure. This is the stark reality of the heart transplant waiting time. The disparity is not random; it is a carefully managed process with life-or-death implications.
In the United States, the United Network for Organ Sharing (UNOS) manages the allocation system. It uses a priority scale from 1 to 6 to determine who gets the next available donor organ. A patient’s status is based on immediate medical need, not simply their place in line.
This system creates a profound gap in outcomes. We will examine the factors behind these critical differences. Our goal is to provide clear, authoritative information to help individuals and families navigate this challenging journey.
Key Takeaways
- The duration on a transplant list varies dramatically, from weeks to several years.
- Medical urgency, not chronological order, is the primary factor for priority.
- Organizations like UNOS use a multi-tiered status system to manage allocations.
- Geographic location and specific biological factors also influence the timeline.
- Understanding the process can help manage expectations during a difficult period.
- Preparation and maintaining health are crucial while awaiting a donor organ.
Introduction: Shocking Realities Behind Heart Transplant Waiting Times
Behind the clinical statistics of cardiac organ allocation lies a human narrative defined by extreme contrasts in the period of anticipation. We observe a system where medical urgency creates vastly different pathways for those in need.
Real Patient Stories and Statistics
The disparity is immediate. A person with the highest priority status may receive an offer within days. Conversely, those on the routine list often face a duration of 18 to 24 months, or longer.
This challenge is even greater for the youngest candidates. Pediatric patients routinely experience extended periods due to the scarcity of size-matched donor organs.
Annually, approximately 3,500 individuals are added to the U.S. list for this procedure. However, only around 3,000 operations are performed. This deficit inevitably prolongs the journey for many.
The Emotional Impact of Waiting
This prolonged uncertainty carries a heavy psychological burden. Individuals and families navigate anxiety and the stress of constant readiness.
Lifestyle becomes restricted. The need to remain near a medical center on short notice is a relentless reality. Understanding these factors is the first step toward managing this difficult experience effectively.
Understanding the Heart Transplant Waiting List
Before placement on the national registry, individuals undergo comprehensive screening to determine eligibility for organ replacement surgery. This systematic approach ensures optimal outcomes for both recipients and the limited donor supply.
How Patients Are Evaluated and Listed
The evaluation process typically spans one to two weeks. Our transplant team conducts thorough assessments across multiple domains.
Key components include:
- Cardiac function tests and comprehensive blood work
- Advanced imaging studies and psychosocial evaluations
- Screening for infectious diseases and cancer risks
This multi-faceted approach determines if a patient’s condition warrants surgical intervention and if they can withstand the procedure successfully.

UNOS Status Levels and Criteria
The United Network for Organ Sharing employs a priority system ranging from Status 1 to 6. Medical urgency drives placement decisions rather than chronological order.
Status 1-3 patients require intensive care unit support with advanced life-sustaining measures. They receive highest priority for available organs. Status 4 individuals may be at home but need intravenous medications or mechanical circulatory devices.
Status 6 encompasses stable candidates who can wait at home without immediate intervention. The transplant team reviews each case weekly, adjusting status levels as medical conditions evolve.
Understanding this classification system helps individuals comprehend their position and set realistic expectations during this challenging period.
Medical Guidelines and Risk Assessments in Transplantation
Evidence-based guidelines from global health organizations establish the framework for determining who qualifies for life-saving cardiac interventions. We follow rigorous protocols to ensure patient safety and optimal outcomes.
ASA/WHO Guidelines and Peer-Reviewed Studies
The American Society of Anesthesiologists and World Health Organization provide standardized criteria for candidate selection. These evidence-based protocols guide our evaluation process.
Recent studies in major transplant journals (2018-2023) show significant improvements. One-year survival rates now exceed 90%, while five-year rates approach 75%. Advances in medications and surgical techniques drive these better outcomes.
Comparative Risk Percentages for Transplant Candidates
We carefully assess risk factors across all major body systems. This includes kidney function, liver health, and pulmonary capacity. The absence of active infections or malignancies is crucial for tolerating immunosuppression.
The evaluation process examines blood type compatibility requirements. Type O patients typically experience longer periods due to limited donor availability. Type AB candidates generally have shorter durations.
| Risk Factor | Surgical Risk | Comparative Context |
|---|---|---|
| Procedure Mortality | 5-8% | Similar to other major cardiac surgeries |
| Status 1-3 Patients Without Intervention | Near-certain mortality | Significantly higher than surgical risk |
| Common Daily Activities | 1 in 10,000 risk | Much lower than surgical procedures |
Our team weighs disease severity against surgical risk. We sometimes recommend additional treatments to optimize patient condition before listing. This approach improves success rates and long-term survival.
A Closer Look at Heart Transplant Waiting Time
The timeline for receiving a compatible organ involves a complex interplay of biological and logistical factors. We examine the key variables that determine how long patients remain on the surgical registry.
Factors Influencing the Waiting Period
Blood type compatibility creates significant disparities in the duration before surgery. Type O patients typically experience 30-40% longer periods than type AB candidates due to universal donor dynamics.
Geographic location substantially impacts availability. Regions with higher donor registration rates offer shorter timelines, while areas with organ shortages create extended delays.
Body size parameters require precise matching. Very large or small patients often face longer periods due to limited availability of appropriately sized donor organs.
The unpredictable nature of donor availability means patients must remain within 4 hours of their medical center. This proximity requirement ensures rapid response when a matching organ becomes available.
| Factor | Impact on Duration | Comparative Example |
|---|---|---|
| Blood Type O | 30-40% longer | Significantly extended period |
| Geographic Region | Varies by 6-18 months | Major regional disparities |
| Body Size Match | Extended for extremes | Limited donor availability |
| VAD Implantation | Additional recovery period | Surgical healing required |
Patients requiring ventricular assist devices experience extended periods due to necessary recovery time. However, these devices enable waiting at home rather than hospitalization.
Understanding these variables helps families prepare for the logistical demands of this critical period. Transplant coordinators maintain 24/7 availability to contact patients immediately when a potential match arises.
Simplifying Complex Medical Terms with Clear Analogies
The intricate world of organ replacement surgery can be demystified through relatable analogies that simplify physiological processes. We translate complex medical terminology into accessible language that resonates with general audiences.
Breaking Down the Transplant Process
Consider the surgical procedure as replacing a failing engine in a vehicle. The diseased organ is removed and replaced with a healthy donor equivalent. This new component must integrate seamlessly with the body’s existing systems.
Surgeons connect the donor organ using vascular attachments similar to plumbing systems. Major blood vessels serve as pipes ensuring proper circulation throughout the body. This connection maintains life-sustaining blood flow to all tissues.
The immune system functions like a sophisticated security network. After transplantation, we carefully adjust this protective system to accept the new organ as friendly rather than foreign. Immunosuppressive medications help maintain this delicate balance.
Ventricular assist devices act as mechanical supports during the interim period. These devices provide circulatory assistance when the native organ cannot function adequately. They serve as bridge supports until a suitable donor becomes available.
While these comparisons simplify complex medical concepts, the actual procedure requires advanced surgical expertise. Our team ensures comprehensive understanding through clear, accessible explanations.
Actionable Checklists for Pre-Surgery Preparation and Recovery
Systematic preparation significantly enhances surgical outcomes and recovery efficiency for patients undergoing major cardiac procedures. We provide comprehensive guidance to optimize readiness and ensure smooth transitions throughout the medical journey.
Steps to Prepare for Heart Transplant Surgery
Thorough pre-operative planning establishes the foundation for successful intervention. Our checklist includes essential actions:
- Arrange temporary housing near the medical facility
- Identify reliable family members for emotional and practical support
- Complete all financial and insurance authorizations in advance
- Maintain optimal health through prescribed medications and lifestyle
- Ensure 24/7 availability for coordinator communications

Essential Recovery Guidelines and Follow-Up
Post-operative care requires disciplined adherence to medical protocols. Patients typically remain hospitalized for two weeks or more following surgery.
- Take three main immunosuppressive medications plus infection prevention drugs
- Attend frequent follow-up appointments during the initial six weeks
- Avoid driving for six weeks while the sternum heals completely
- Gradually return to work within two to three months based on recovery progress
- Manage incision discomfort with prescribed pain medication as needed
Practical Advice for Staying Within Proximity to Care
Geographic requirements are critical during the recovery phase. Patients must remain within 30 minutes of the medical center for the first six weeks after discharge.
- Social workers assist with affordable guest housing arrangements
- Family support is encouraged through open visiting hours
- Sick visitors must be prohibited to protect patient health
- Support groups provide valuable connection with others sharing similar experiences
- Full recovery typically occurs within three to six months with proper care
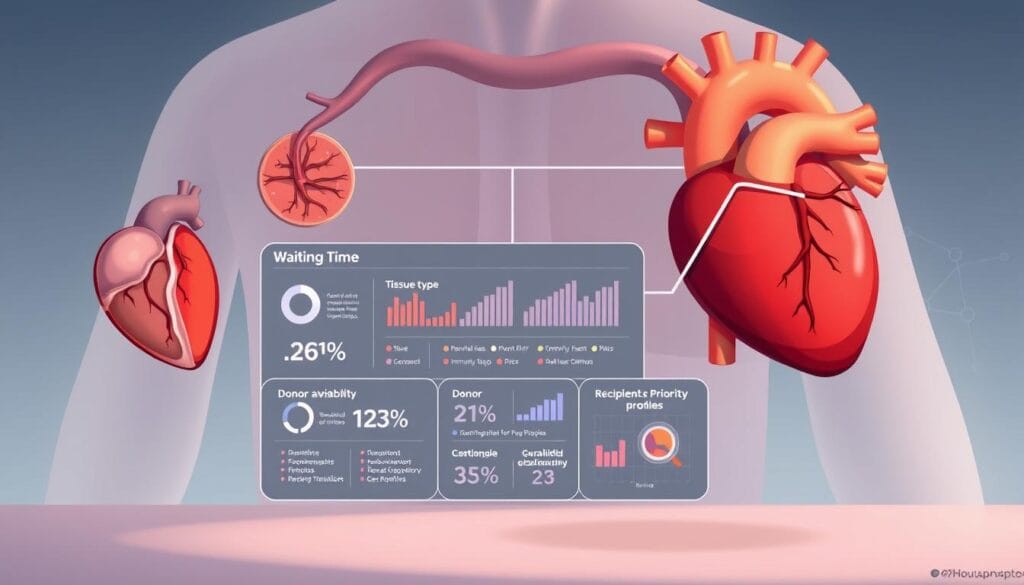
Visual Tools and Data-Driven Infographics
Visual data representations transform complex medical allocation processes into accessible insights for candidates and families. We employ comprehensive graphical tools to clarify the intricate factors influencing surgical readiness.
Comparison Tables and Symptom Timelines
Our comparison tables display durations across different priority levels. Status 1-3 individuals typically receive offers within days to weeks. Status 4 candidates may wait weeks to months. Status 6 patients often face extended periods of 18-24 months.
Visual timelines map the entire journey from evaluation through long-term follow-up. These tools help set realistic expectations for each phase. Symptom progression charts empower individuals to recognize changes requiring medical attention.
Infographic Elements to Clarify the Procedure
Geographic availability charts illustrate regional variations in organ supply. Blood type comparison graphics show how type O candidates experience longer durations than type AB patients.
Procedure diagrams simplify complex surgical concepts through clear visual explanations. Outcome charts present survival rates at 1, 5, and 10-year intervals based on peer-reviewed data.
These mobile-friendly visual tools provide immediate comprehension of critical information. They support informed decision-making throughout the medical journey.
Frequently Asked Questions About Heart Transplant Waiting Lists
Patients and families navigating the organ allocation process often have pressing questions about eligibility, timelines, and life after surgery. We address the most common concerns to provide clarity during this challenging journey.
How do I know if I need this procedure? Individuals with severe cardiac conditions unresponsive to conventional treatments may benefit. Cardiologists refer appropriate candidates for comprehensive evaluation by our specialized team.
What happens when a donor organ becomes available? The coordinator contacts patients immediately. They must reach the hospital within the designated window for final assessments before proceeding.
Consult your medical team if experiencing significant symptoms. Request referral to accredited centers for proper evaluation. This information aligns with guidelines from leading cardiac associations.
Share this guide with others facing similar health challenges. Knowledge empowers better decisions during complex medical processes.
FAQ
What is the average wait for a donor organ?
The duration varies significantly based on a patient’s status level, blood type compatibility, body size, and geographic location. Some individuals may receive an offer in weeks, while others remain on the list for years.
How does the transplant team decide who gets the next available organ?
The system prioritizes patients based on medical urgency, not simply the length of time they have been waiting. The sickest individuals, as determined by specific clinical criteria and tests, receive top priority for a matching donor heart.
What can a patient do to improve their position on the list?
A person cannot directly move up the list. However, following all medical advice, taking prescribed medications, and maintaining overall health can help ensure they remain a viable candidate when a match is found.
What are the primary risks associated with this life-saving procedure?
The primary risks include organ rejection, infection, and side effects from necessary immunosuppressant drugs. The transplant team carefully weighs these risks against the dangers of end-stage heart disease.
How does a patient’s blood type affect their wait?
Blood type matching is crucial. Patients must receive an organ from a donor with a compatible type. This requirement can create longer wait times for individuals with less common blood types.
What support is available for families during the waiting period?
Most hospitals offer extensive support services, including social workers, support groups, and counseling. These resources help patients and their loved ones manage the emotional stress of the journey.