Diverticulitis is a common issue that affects 67% of adults in the U.S. over their lifetime. This shows we need new ways to handle this condition. The link between the gut microbiome and diverticulitis is key to finding these solutions.
The gut microbiome is full of trillions of microorganisms that are vital for our health. They help keep us healthy and can affect our risk of diseases like diverticulitis. By studying how the gut microbiome and diverticulitis are connected, doctors can find new ways to prevent and treat the condition. This could greatly improve life for those with diverticulitis.
Key Takeaways
- Diverticulitis affects a significant portion of the adult population in the United States.
- The gut microbiome plays a crucial role in maintaining overall health and can influence the development of gastrointestinal disorders.
- Understanding the relationship between the gut microbiome and diverticulitis is essential for developing targeted interventions.
- Modulating the gut microbiome may hold the key to preventing and managing diverticulitis.
- Exploring the potential of probiotics and dietary interventions in microbiome modulation is a promising avenue for diverticulitis prevention.
Introduction to Diverticulitis and the Gut Microbiome
Diverticulosis is when small pouches (diverticula) form in the colon. It’s common, affecting about 67% of adults at some point. If these pouches get inflamed, it’s called diverticulitis. This can cause belly pain, fever, and other stomach issues.
What causes diverticulitis isn’t clear, but eating less fiber, being overweight, and aging can increase the risk.
Understanding Diverticulitis and its Prevalence
Many people get diverticular disease, a common gut issue. It’s found in up to 25% of people over 40. In Italy, a meeting found that by age 70, over half the population has it.
The Role of the Gut Microbiome in Human Health
The gut microbiome is a key area to study for diverticulitis. It’s full of different microorganisms that help keep us healthy. They affect our immune system, how we absorb nutrients, and make important substances.
Changes in these microorganisms, called dysbiosis, can lead to many gut problems. This includes inflammatory bowel diseases, irritable bowel syndrome, and diverticulitis. Studying how the gut microbiome and diverticulitis interact could lead to new treatments.
The Etiology of Diverticulitis and Microbiota Alterations
The exact cause of diverticulitis is still a mystery, but it likely involves diet, lifestyle, genes, and the gut microbiome. Studies show that changes in the gut microbiome, or dysbiosis, might be key in causing and worsening diverticulitis.
This imbalance in the gut can lead to inflammation, weaker gut walls, and a higher chance of getting diverticulitis. We need more research to understand how these microbiota changes affect diverticulitis.
Recent studies have uncovered some important facts about the gut microbiome and diverticulitis:
- Screening endoscopies show diverticula in about 33% of people aged 50 to 59 and 71% of those over 80 who don’t show symptoms.
- Studies on twins show that 40 to 53% of the risk of diverticular disease comes from genetics.
- An analysis of 535 people without symptoms found no big differences in their gut microbiota with or without diverticulosis.
- Using antibiotics doesn’t help more than a placebo in treating uncomplicated diverticulitis.
| Statistic | Finding |
|---|---|
| Diverticula prevalence | 33% in 50-59 year olds, 71% in over 80s |
| Heritable risk factors | 40-53% of individual risk |
| Microbiome in asymptomatic diverticulosis | No strong differences compared to controls |
| Antibiotics in uncomplicated diverticulitis | No improvement over placebo |
These studies hint that the gut microbiome might be involved in diverticulitis, but we don’t know the exact details. More research is needed to understand how the gut microbiome, host factors, and diverticulitis are connected.
Gut Microbiota Composition in Asymptomatic Diverticulosis
A recent study looked at the gut microbiota and inflammation in people with and without diverticulosis. It used colonoscopy patients without diverticular or inflammatory bowel disease. The study had two groups: those with and without diverticulosis.
Study Design and Participant Selection
Biopsies were taken from the colon. The study analyzed gut microbiota with advanced methods like the IS-pro microbiota assay. It used cosine distance analysis and diversity analysis to compare microbiota profiles. A PLS-DA model helped predict group membership by microbiota.
Microbiota Analysis Techniques and Data Interpretation
The study found similar gut microbiota in all individuals, with or without diverticula. There were no big differences in diversity or inflammation markers. This suggests the gut microbiome and inflammation don’t greatly affect diverticula formation.
Some bacteria like Bifidobacterium pseudocatenulatum and Prevotella copri were more common in the control group. On the other hand, Roseburia intestinalis, Dorea sp. CAG:317, and Clostridium sp. CAG: 299 were found more in the diverticulosis group. These findings hint that the gut microbiome might influence diverticula development and progression.
“The results showed that the gut microbiota profiles were highly similar within individuals, regardless of the presence or absence of diverticula.”
Diverticulitis, microbiome modulation, and Mucosal Inflammation
The study on asymptomatic diverticulosis didn’t show big differences in gut bacteria or inflammation between those with and without diverticula. Yet, the gut microbiome’s role in diverticulitis is still being studied. Research now points to its possible role in diverticulitis. This includes causing inflammation, changing the gut lining, and letting harmful bacteria grow.
It’s key to understand how the gut microbiome, inflammation, and diverticular disease interact. This knowledge can help create new treatments for diverticulitis. Studies show that the bacteria in the lining of the gut are different in people with and without inflamed diverticula. Inflamed areas have more Microbacteriaceae and Ascomycota.
People with diverticular disease that causes symptoms have more Enterobacteriaceae and less Bacteroides/Prevotella and Akkermansia than healthy people. Inflamed diverticula have more bacteria and a higher F/B ratio. This suggests that an imbalance of gut bacteria might help cause diverticulitis.
“Understanding the complex interplay between the gut microbiome, inflammation, and diverticular disease is crucial for developing targeted interventions to prevent and manage diverticulitis.”
Research is ongoing to better understand the link between the gut microbiome and diverticular disease. The goal is to find new treatments and ways to prevent it. By learning more about how gut bacteria affect diverticulitis, doctors can improve treatment and help patients more.
The Gut Microbiome and Diverticulitis: Insights from Research
Recent studies have uncovered a link between the gut microbiome and diverticulitis. They show that people with diverticulitis have different gut bacteria than those without it. This imbalance, or dysbiosis, includes fewer types of bacteria, more harmful ones, and fewer helpful ones.
Microbial Dysbiosis and Diverticulitis Risk
This imbalance might lead to more inflammation, a weaker gut lining, and a higher chance of diverticular problems. For example, some studies found more of certain bacteria like Coriobacteria, Anaerotruncus, Subdoliganulum, Marvinabryantia, and Akkermansia in those with diverticulitis. But, there were fewer Barnesiella and Coprococcus bacteria.
Also, the alpha diversity (a way to measure bacterial variety) was higher in those with diverticulitis at diagnosis. But, this wasn’t a statistically significant finding. This means certain gut bacteria might make people more likely to get diverticulitis.
We need more research to prove that gut bacteria directly cause diverticulitis. If we find this link, it could lead to new treatments that target the gut microbiome for prevention and treatment.
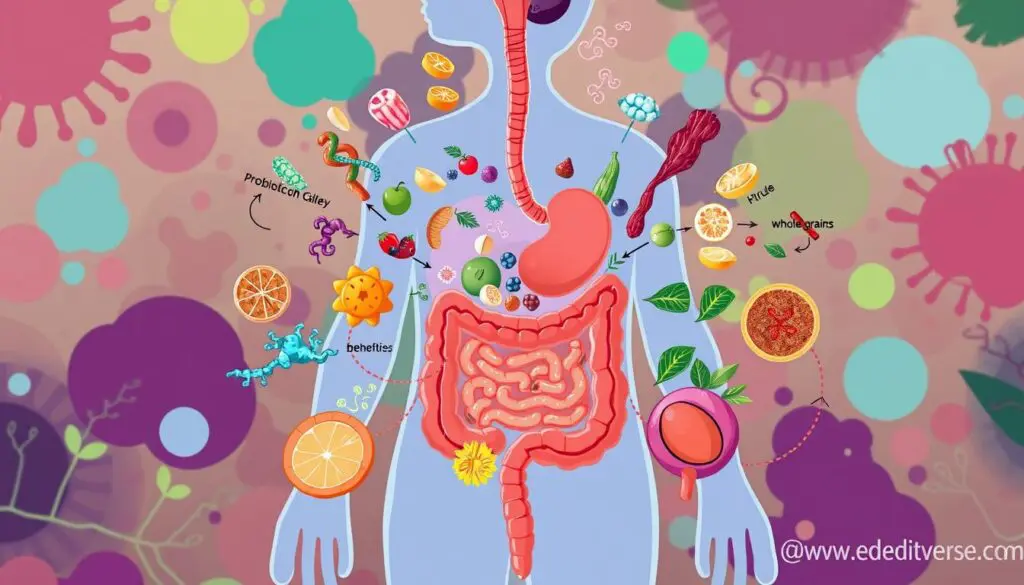
Probiotics and Dietary Interventions for Microbiome Modulation
Studies show that the gut microbiome might play a big part in diverticulitis. So, trying to change the gut bacteria could help prevent and manage the disease. Probiotics, which are good bacteria, can help balance the gut and lessen inflammation.
Also, eating more fiber can change the gut bacteria and might lower the risk of diverticulitis. Researchers are looking into how probiotics and diet can help with diverticular disease. This could lead to new ways to treat it in the future.
Probiotics for Gut Microbiome Modulation
Many studies have looked into using probiotics for diverticulitis. One study found that taking Limosilactobacillus reuteri ATCC PTA 4659 helped with acute diverticulitis. People taking the probiotic had less pain, stayed in the hospital less, and had lower inflammation markers.
Dietary Interventions for Gut Health
Eating more fiber is another way to help the gut microbiome. Fiber feeds the good bacteria in our gut, keeping it healthy. This could lower the risk of diverticulitis.
| Probiotic Strain | Key Findings |
|---|---|
| Limosilactobacillus reuteri ATCC PTA 4659 |
|
Using probiotics and diet together can help manage diverticulitis. Doctors can use this approach to improve gut health. More research is needed, but it could lead to better treatments.
“The gut microbiome is a complex and dynamic ecosystem that plays a crucial role in human health, and understanding its relationship with diverticular disease is an exciting frontier in modern medicine.”
The Role of Antibiotics in Diverticulitis Management
Antibiotics were once a key part of treating acute diverticulitis. The aim was to fight the infection thought to be present. But, new studies have raised doubts about their effectiveness. They show that overusing antibiotics can harm the gut’s balance, leading to more problems and a higher chance of the condition coming back.
Reconsidering Antibiotic Use in Diverticulitis
Now, doctors are thinking differently about antibiotics for diverticulitis. They’re moving towards less invasive treatments that focus on supporting the body. This change is based on research that suggests targeted antibiotic use can be better. It helps keep the gut’s balance and lowers the risk of the condition returning.
Probiotics, like Lactobacillus and Bifidobacterium, are being seen as helpful in preventing and treating diverticulitis. These probiotics can lessen inflammation by affecting certain proteins in the body.
Researchers are also looking at different mixes of antibiotics and probiotics in animals. They want to find the best way to prevent and treat diverticulitis. They’re testing various amounts of these treatments in rats to see what works best.
As we learn more about the gut microbiome and diverticulitis, doctors are changing how they use antibiotics. They’re looking at ways to keep the gut healthy without harming it. This new approach aims to manage diverticulitis more effectively.
Microbiome-Targeted Therapies for Diverticulitis Prevention
Researchers are now looking into new treatments for diverticulitis. They aim to change the gut bacteria to prevent more cases. These treatments might include special probiotics, transplanting healthy gut bacteria, and eating foods that help good bacteria grow.
These methods aim to fix the balance of gut bacteria. This could help stop diverticulitis from happening or coming back. Scientists are checking if these new treatments are safe and work well.
Probiotics for Diverticulitis Prevention
Some probiotics, like Lactobacillus reuteri, could help with gut health. Studies show L. reuteri can fight off bad bacteria and ease symptoms in some conditions. It might also help prevent diverticulitis.
Fecal Microbiota Transplantation (FMT)
Fecal microbiota transplantation means adding healthy bacteria from someone else to your gut. Early studies suggest it can clear up diverticulitis. This method could be a new way to fix the gut bacteria balance.
Dietary Modifications
Eating more fiber and foods like yogurt can help good gut bacteria grow. This could lower the risk of getting diverticulitis. By eating right, you can change your gut bacteria for the better.
More research is needed, but these new treatments could be big steps forward. They might help doctors treat diverticulitis better. This could make a big difference for patients.
“The gut microbiome was the leading factor explaining variance in the metabolomics profile (R2 = 22.4%).”
Lifestyle Factors and the Gut Microbiome in Diverticulitis
Lifestyle choices like what we eat and how active we are affect our gut microbiome and gut health. A study showed that eating a lot of fiber makes our gut microbiome diverse and strong. This can help prevent diverticulitis. Also, exercising regularly helps our gut microbiome stay healthy.
Diet, Exercise, and Microbiome Influence
Knowing how our lifestyle affects our gut microbiome and diverticulitis risk helps us make better choices. Eating foods high in fiber, like fruits, veggies, and whole grains, can make our gut microbiome strong. This can protect us from getting diverticulitis. On the other hand, eating a lot of processed foods can make our gut microbiome less diverse, raising our risk of diverticulitis.
Exercise also helps our gut microbiome. It encourages the growth of good bacteria and helps make our intestines healthy. By understanding how our lifestyle affects our gut microbiome, we can make choices that support our gut health and lower our risk of diverticulitis.

“Understanding the complex interplay between lifestyle factors, the gut microbiome, and diverticulitis risk can inform holistic approaches to prevention and management.”
Future Directions in Gut Microbiome Research for Diverticulitis
Our understanding of the gut microbiome’s role in diverticulitis is growing. Longitudinal studies can track how the gut microbiome changes over time. They can show how it affects diverticular disease.
Looking into specific microbes that might raise the risk of diverticulitis could help make new diagnostic tools. Exploring how changing the gut microbiome with probiotics or diet can help prevent diverticulitis is also key. Working together, doctors, microbiologists, and researchers can make new strategies to improve diverticulitis treatment.
- Longitudinal studies tracking gut microbiome changes over time and their link to diverticular disease development and progression
- Identification of microbial signatures or biomarkers associated with diverticulitis risk to inform diagnostic and predictive tools
- Investigations into the mechanisms of gut microbiome modulation through probiotics, dietary interventions, and fecal microbiota transplantation for diverticulitis prevention and management
- Interdisciplinary collaboration between clinicians, microbiologists, and researchers to advance knowledge and translate findings into effective, microbiome-based strategies for diverticular disease
| Research Focus | Potential Impact | Existing Evidence |
|---|---|---|
| Longitudinal studies on gut microbiome changes and diverticular disease | Provide valuable insights into the role of the gut microbiome in the development and progression of diverticular disease | A study found that specific microbial signatures were associated with the presence of diverticular disease |
| Identification of microbial biomarkers for diverticulitis risk | Enable the development of diagnostic and predictive tools for diverticulitis | Research has shown that certain microbial species or community profiles may be linked to an increased risk of diverticulitis |
| Gut microbiome modulation for diverticulitis prevention and management | Explore effective, microbiome-based strategies for improving outcomes in diverticular disease | Studies have suggested that interventions like probiotics, dietary changes, and fecal microbiota transplantation may influence the prevention and management of diverticulitis |
“Collaboration between clinicians, microbiologists, and researchers will be key in advancing our knowledge and translating these findings into effective, microbiome-based strategies for improving outcomes in diverticular disease.”
Conclusion
The study of the gut microbiome and its role in diverticulitis is growing. It shows promise for better prevention and treatment of this common gut issue. Even though the first study didn’t find big changes in gut bacteria, more research is needed.
Studies are looking into new treatments like probiotics and changes in diet. They also want to rethink how antibiotics are used. These efforts aim to help doctors find new ways to keep the gut healthy and lessen the impact of diverticulitis.
More research is needed to fully understand how the gut microbiome affects diverticulitis. As we learn more, doctors will be able to create treatments that focus on the gut microbiome. This could lead to better care for people with this condition.
FAQ
What is the role of the gut microbiome in the development and progression of diverticulitis?
Studies show that changes in the gut microbiome, or dysbiosis, might affect diverticulitis. This imbalance can cause inflammation and make the gut more prone to infection.
Do individuals with asymptomatic diverticulosis have different gut microbiota profiles compared to those without diverticula?
Research suggests that people with or without diverticula have similar gut microbiota. There’s no big difference in inflammation or microbiota diversity between the two groups. This means the gut microbiome might not be a key factor in forming diverticula.
How can probiotics and dietary interventions help modulate the gut microbiome in the context of diverticulitis?
Probiotics can help balance the gut bacteria and reduce inflammation. Eating more fiber can also change the gut microbiome and might lower the risk of diverticulitis. Scientists are studying how these methods can help manage diverticulitis.
What is the role of antibiotics in the management of diverticulitis, and how is this being reconsidered?
Antibiotics were once a go-to for treating diverticulitis, but their use is being reevaluated. Overusing antibiotics can harm the gut microbiome, leading to more problems and higher recurrence rates. Now, doctors are looking at less invasive treatments to protect the gut’s balance.
How can lifestyle factors, such as diet and exercise, influence the gut microbiome and the risk of diverticulitis?
Eating a lot of fiber can make the gut microbiome more diverse and strong, which might help prevent diverticulitis. Exercise also benefits the gut microbiome, keeping the intestines healthy. These lifestyle choices can play a big part in lowering the risk of diverticulitis.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8423250/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11172644/
- https://immunogenetics.nl/wp-content/uploads/2021/10/2_2011probiotics2011.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10011305/
- https://www.nature.com/articles/s41467-024-47859-4
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9946712/
- https://link.springer.com/article/10.1007/s10620-022-07600-x
- https://www.mdpi.com/1422-0067/23/23/14799
- https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-024-01374-9
- https://www.medrxiv.org/content/10.1101/19001404v1.full
- https://www.jgld.ro/jgld/index.php/jgld/article/download/277/145/
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0256657
- https://www.mdpi.com/2075-1729/12/12/2129
- https://arts.units.it/retrieve/38761321-0090-45ac-9264-762dc5608dc9/PICCIN A 2023 Diverticular disease and rifaximin.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8070761/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8398895/
- https://www.gutmicrobiotaforhealth.com/probiotics-with-an-anti-inflammatory-effect-may-reduce-abdominal-pain-and-hours-of-hospitalization-in-adult-patients-with-acute-uncomplicated-diverticulitis/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10044695/
- https://link.springer.com/article/10.1007/s10787-022-01093-w
- https://www.mdpi.com/1648-9144/57/8/802
- https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1225120/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10957260/
- https://www.mdpi.com/2075-4426/12/9/1520
- https://www.mdpi.com/2079-6382/12/3/443
- https://academic.oup.com/bjsopen/article/8/3/zrae032/7686311