“The true sign of intelligence is not knowledge but imagination.” – Albert Einstein
3D imaging technology has changed oral surgery, especially in planning surgeries. Now, with cone beam computed tomography (CBCT) and other tools, doctors can use volumetric data for better surgical plans. This article looks at the newest research and methods in 3D imaging for oral surgery. It shows how these new ways are changing how doctors handle complex surgeries.
Key Takeaways
- 3D imaging, especially CBCT, is key in oral surgery for planning before surgery and simulating surgeries virtually.
- 3D printed models and guides help make complex surgeries like orthognathic surgery and removing bone tumors more accurate.
- Techniques like CAD/CAM are changing craniomaxillofacial surgery. They allow for planning surgeries virtually and making implants for each patient.
- Using 3D imaging, planning virtually, and 3D printing has made surgeries better and reduced complications after surgery in many oral and maxillofacial procedures.
- Research is ongoing to make 3D imaging and computer-assisted surgery more accurate, efficient, and useful in oral and maxillofacial surgery.
Traditional Methods versus 3D Surgical Planning
Traditional surgical planning has been the norm in oral and maxillofacial surgery. But, 3D imaging and planning have brought a new level of precision and predictability. Studies now show that 3D surgical planning, or virtual surgical planning (VSP), is more accurate and leads to better results than old methods.
Comparison of Accuracy and Outcomes
VSP cuts down the time needed for planning by a lot. It also makes surgical accuracy better, with errors less than 2 mm. A study found VSP can shorten planning time by up to 30%.
When looking at VSP systems like Dolphin Imaging and IPS Case Designer, Dolphin Imaging outperformed in many ways. But IPS was easier to use, needing fewer windows for planning.
Limitations of Traditional Surgical Planning
Old planning methods struggle to fully see the complex 3D anatomy. They also face challenges in making the plan work in real surgery. Even with 3D planning, picking the best prediction models is still up for debate.
| Metric | Traditional Surgical Planning | 3D Surgical Planning |
|---|---|---|
| Accuracy | Limited due to 2D visualization | Improved accuracy with 3D visualization |
| Planning Time | Longer planning time | Reduced planning time by up to 30% |
| Surgical Outcomes | Potential challenges in translating the plan | Better overall surgical outcomes |
Computer-Aided Design and Manufacturing in Craniomaxillofacial Surgery
The use of computer-aided design (CAD) and computer-aided manufacturing (CAM) has changed craniomaxillofacial surgery a lot. These digital tools help make surgical guides, models, and implants that fit each patient perfectly. This leads to more accurate and tailored surgeries. With CAD/CAM, doctors can now plan and do complex surgeries with much more precision. This means better results for patients and fewer risks.
A review looked into how CAD/CAM technology helps with placing craniofacial implants and making ear prosthetics. It looked at 16 studies with 30 cases. The studies used CT scans, 3D scanners, and laser scanners to gather data. Software like Ease Orbital Implant Planning and Geomagic was used to make custom surgical tools and implants.
| Preoperative Data Collection | Digital Designing Software | Surgical Outcomes |
|---|---|---|
|
|
|
CAD/CAM technology has been used in craniomaxillofacial surgery for over 15 years. It helps place implants with great precision using custom guides. These digital methods make dental implant placement more precise. They also cut down on patient visits, lab time, and fabrication steps without hurting the results.
“CAD/CAM technology claims to reduce patient appointments, clinical and laboratory times, and the steps of fabrication without compromising clinical outcomes.”
The review shows how computer-aided design and computer-aided manufacturing are becoming more popular in craniomaxillofacial surgery. They help make implants and guides that fit each patient perfectly. This leads to more precise surgeries and better results for patients.
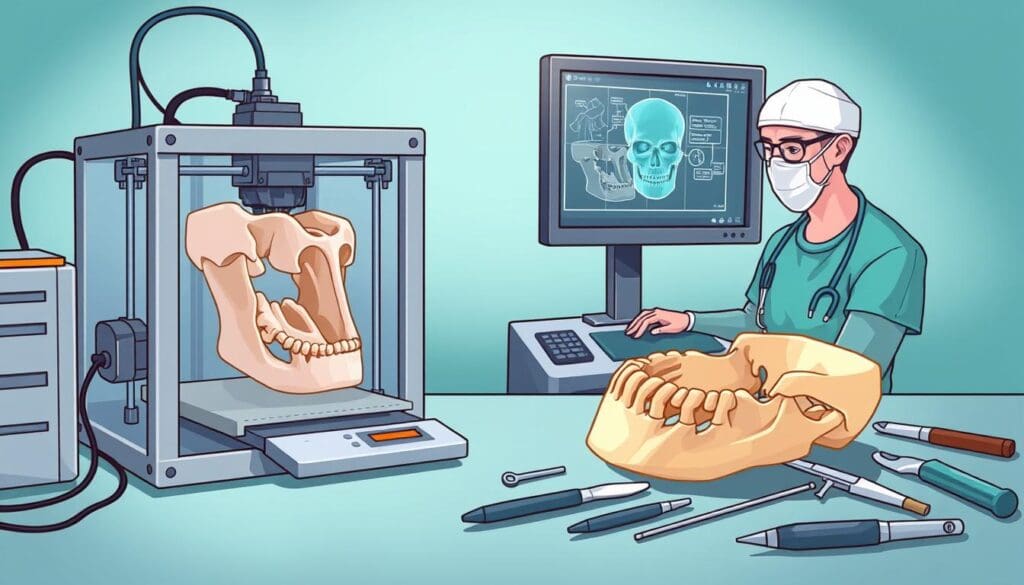
Role of 3D Printing in Surgical Planning
The advent of 3D printing has changed how surgeons plan surgeries, especially in oral and maxillofacial surgery. This technology lets doctors make patient-specific 3D printed models that look just like the patient’s body parts. These models are key in planning surgeries, helping make custom surgical guides and implants.
Patient-Specific 3D Printed Models
Patient-specific 3D printed models have greatly helped in orthognathic surgery. This surgery needs precision and accuracy. These models let surgeons plan and practice complex surgeries, leading to better results and shorter surgery times. They help surgeons see potential problems, try out surgical steps, and make custom guides and implants.
Applications in Orthognathic Surgery
3D printing has changed orthognathic surgery for the better. Doctors can now make 3D printed models that show exactly what they’ll be working on. This makes their surgeries more precise and predictable. These models help make customized surgical guides and implants that fit each patient perfectly, leading to better results.
“The use of 3D printing technology in surgical planning has been a transformative development, particularly in the field of orthognathic surgery. By creating patient-specific 3D printed models, we can now plan and execute complex procedures with unprecedented accuracy, leading to improved patient outcomes and reduced surgical times.”
3D printing has changed how surgeons plan complex surgeries. It lets them make patient-specific 3D printed models for planning and performing surgeries with great precision. This leads to better care and outcomes for patients.
3D Imaging Research in Oral Surgery: Interpreting Volumetric Data for Surgical Planning
3D imaging tech, especially cone beam computed tomography (CBCT), has changed oral surgery. It gives doctors detailed 3D views of the mouth and jaw area. This helps them plan surgeries better by seeing the complex anatomy.
They can make virtual surgical plans that are more precise. This leads to better results for patients.
Orthognathic surgery used to be tough, needing big surgeries and bone grafts. These methods could cause problems like infection or nerve damage. But, 3D tech helps doctors see better during surgery. This can make recovery faster and less painful.
3D printing has also changed medical procedures. There are different methods, each with pros and cons. SLA gives great details but takes a long time and has few materials. FDM is fast and cheap but the results might not be as strong.
SLS makes custom implants that are strong and fit well with the body. But, it’s slow and expensive.
| 3D Printing Technique | Advantages | Limitations |
|---|---|---|
| Stereolithography (SLA) | High resolution, clean surface finishes | Long processing times, limited material choice |
| Fused Deposition Modeling (FDM) | High production speed, cost-effectiveness | Reduced strength and durability, manual removal of support structures |
| Selective Laser Sintering (SLS) | Patient-specific implants, high biocompatibility and mechanical strength | Time-consuming, costly |
Using 3D imaging and printing, doctors can make surgeries more precise. This leads to better results, fewer problems, and happier patients in oral and maxillofacial surgery.
“The advent of 3D technology has revolutionized the way we approach surgical planning, allowing us to visualize and analyze the complex anatomy of the oral and maxillofacial region with unprecedented detail.”
Virtual Surgical Planning for Orthognathic Surgery
The use of virtual surgical planning has changed how we do orthognathic surgery. Now, doctors use 3D images and special software to plan surgeries online. They use CBCT scans, digital dental models, and advanced tools to plan how to move the jaws and other parts.
Digital Workflow and Virtual Planning Process
This planning helps spot problems, improve surgery results, and make custom guides and devices. It makes the whole computer-aided surgery process smoother. Doctors can see and change 3D body parts, try out different surgery plans, and make the best treatment plan before surgery.
| Key Steps in Virtual Surgical Planning | Description |
|---|---|
| 1. 3D Imaging and Dental Scanning | Capture comprehensive 3D data using CBCT scans and digital dental impressions |
| 2. Virtual Planning and Simulation | Use special software to plan the surgery in 3D, including moving jaws and soft tissues |
| 3. Customized Surgical Guides | Make patient-specific guides and devices to help with the surgery |
This digital workflow makes orthognathic surgery more precise and predictable. It leads to better results and happier patients.
“Virtual surgical planning has changed how we do complex orthognathic procedures. It helps us make the best treatment plans and ensures surgery is done right.”
Accuracy of Virtual Planning Techniques
The accuracy of virtual planning techniques in orthognathic surgery has been studied a lot. Research shows that computer-aided surgery makes jaw repositioning more precise than old methods. By using digital workflows and new software, doctors can simulate surgeries very accurately. This leads to better surgical outcomes and fewer risks.
Virtual planning helps place the jaws just right. This is key for stable bites and the best looks and function for the patient.
Precision of Jaw Repositioning
A study looked into how accurate virtual planning is in orthognathic surgery. It focused on how well jaw repositioning works. Researchers made 3D models for planning and after surgery, then checked how close they matched.
The study found a highly statistically significant degree of agreement between before and after surgery. This means the method was very reliable (ICC = 0.9).
“The color-coded map indicated distances between the postoperative model and virtual planning model, with positive colors representing areas in front of the reference surface and negative colors indicating areas behind the reference surface.”
This study showed how important the ICP algorithm and color maps are for checking accuracy in orthognathic surgery. These tools have greatly improved the accuracy of virtual planning and precision of jaw repositioning in surgeries.

Computer-Assisted Orthognathic Surgery for Cleft Lip/Palate
Computer technology has changed how we treat cleft lip and/or palate. Using 3D imaging, virtual planning, and guides, doctors can fix complex problems better.
This new way helps move jaws into the right place, improve looks, and make eating easier. It makes life better for those with cleft lip and palate. The incidence of cleft lip and palate ranges from 1.0/1000 to 2.2/1000, with higher prevalence seen in the Asian population.
Computer-assisted surgery is especially good for those with cleft lip and palate. Studies show that 9% to 60% of these patients need this surgery. This shows how important this new method is.
| Metric | Value |
|---|---|
| Mean Age of Patients | 18.5 years (range: 15.3 to 25.7 years) |
| Average Preoperative Orthodontic Treatment Duration | 8.8 months |
| SNA Angle Deviation from Normative Data | Significantly smaller |
| A-N Perpendicular Distance (One-Jaw Design) | 2.66 mm |
Thanks to virtual surgical planning and patient-specific surgical guides, doctors can now fix complex face problems with great accuracy. This makes a big difference in the lives of those with cleft lip and/or palate.
Evolving Management of Dentofacial Deformities with Digital Planning
The way we handle dentofacial deformities has changed a lot with digital planning. Now, with 3D imaging and virtual surgical planning, doctors can fix complex cases better. They use patient-specific guides and devices for this.
This new method lets doctors make custom guides and models for each patient. Thanks to digital planning techniques, surgeries are now more precise and predictable. This has made care for dentofacial deformities better.
Studies show that 3D models are great for learning and training in healthcare. They help spot and understand dentofacial deformities well.
Cone beam computed tomography (CBCT) and 3D printing have improved a lot in orthognathic surgery. They help with detailed planning and making virtual models of the face.
Using 3D technology in surgeries can lead to better results. It helps reduce surgery time and how long patients stay in the hospital.
| Metric | Value |
|---|---|
| Total Articles Analyzed | 8 |
| Total Subjects Included | 5,552 |
| Gender Distribution | 44.56% Male, 55.43% Female |
| Age Range | 14.7 to 56 years |
| Ethnicity Distribution | 3 studies from Korea, 2 from China, 1 from the United States |
| Skeletal Class Distribution | Higher frequency of skeletal class III deformities compared to class II, with some class I and facial asymmetry |
| Software Used | Python, R, and unspecified software |
| Machine Learning Models | Convolutional neural network ResNet, DenseNet with stochastic gradient descent |
In conclusion, digital planning techniques have changed how we handle dentofacial deformities. Now, doctors can give patients more tailored and effective surgery.
Conclusion
3D imaging and advanced tech have changed oral surgery for the better. Now, with tools like cone beam CT, computer-aided design, and 3D printing, surgeons can plan surgeries with great accuracy. This leads to more precise and tailored treatments for patients.
Virtual planning and digital workflows have made handling complex cases easier. This is true for things like fixing jaw problems and correcting cleft lip/palate issues. Thanks to these advances, surgeries are more effective and patient care is better.
As tech keeps getting better, the future of oral surgery looks bright. We can expect better care, better results, and a better life for those with dental issues. The use of 3D imaging and digital tools has changed how surgeries are planned. This means surgeries are now more accurate and focused on what’s best for the patient.
Technologies like cone beam CT and 3D printing let surgeons work with detailed images. This helps them manage tough dental and facial problems better. As these technologies grow, we can look forward to more progress in patient care and outcomes. This will improve the lives of those dealing with dental and facial issues.
FAQ
What is the role of 3D imaging research in oral surgery?
3D imaging technology, like cone beam computed tomography (CBCT), has changed oral surgery. It gives doctors detailed 3D views of the mouth and jaw area. This helps with better surgical planning and understanding complex anatomy.
How does 3D surgical planning compare to traditional methods?
3D surgical planning is more accurate in moving the jaw and leads to better results. Yet, traditional methods have limits. They can’t fully show the 3D anatomy and might struggle to match the planned surgery with reality.
What role do computer-aided design and manufacturing play in craniomaxillofacial surgery?
Computer-aided design (CAD) and manufacturing (CAM) have changed craniomaxillofacial surgery. They help make surgical guides, models, and implants specific to each patient. This leads to more precise and tailored surgeries.
How is 3D printing being used in surgical planning?
3D printing is key in surgical planning, especially in oral and maxillofacial surgery. It makes accurate, patient-specific models. These models help with detailed surgical planning and making custom guides and implants.
How has virtual surgical planning enhanced the approach to orthognathic surgery?
Virtual surgical planning has improved orthognathic surgery. It uses 3D imaging and software for detailed planning and simulation. This process helps plan jaw repositioning with precision, using CBCT scans and digital models.
What is the accuracy of virtual planning techniques in orthognathic surgery?
Virtual planning makes jaw repositioning more precise than traditional methods. Digital tools and software help simulate surgeries accurately. This leads to better results and fewer complications.
How have computer-assisted technologies improved the management of orthognathic surgery for patients with cleft lip and/or palate?
Computer-assisted technologies have greatly improved surgery for cleft lip and/or palate patients. 3D imaging and virtual planning help tackle complex anatomy challenges more effectively.
How has the integration of digital planning transformed the management of dentofacial deformities?
Digital planning has changed how dentofacial deformities are managed. It uses 3D imaging and virtual planning for precise and predictable results. This approach makes custom surgical guides and devices for each patient’s needs.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10389328/
- https://www.quintessence-publishing.com/usa/en/product/cone-beam-volumetric-imaging-in-dental-oral-and-maxillofacial-medicine
- https://jkamprs.springeropen.com/articles/10.1186/s40902-023-00409-2
- https://www.mdpi.com/2076-3417/11/3/1009
- https://www.ejomr.org/JOMR/archives/2023/1/e1/v14n1e1.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8582823/
- https://link.springer.com/article/10.1007/BF01660745
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8953417/
- https://www.intechopen.com/chapters/85579
- https://threedmedprint.biomedcentral.com/articles/10.1186/s41205-022-00142-y
- https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1347107/full
- https://www.mdpi.com/2076-3417/13/17/9907
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10170664/
- https://head-face-med.biomedcentral.com/articles/10.1186/s13005-020-00250-2
- https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-023-02811-8
- https://www.mdpi.com/2076-3417/12/9/4305
- https://link.springer.com/chapter/10.1007/978-981-15-1346-6_41
- https://www.mdpi.com/2076-3417/12/9/4461
- https://www.mdpi.com/2075-4426/14/6/647
- https://www.europeanreview.org/wp/wp-content/uploads/7858-7865.pdf
- https://www.mdpi.com/2076-3417/13/2/1226
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7452983/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6631689/